The inhalation of asbestos, a group of naturally occurring silicate minerals with a fibrous structure, has long been a concern for public health and occupational safety. The lungs, our vital organs of respiration, are equipped with sophisticated defense mechanisms to counteract foreign particles’ intrusion, including asbestos fibers. However, the peculiar characteristics of these fibers present a unique challenge to the pulmonary clearance system. This essay investigates the intricate physiological mechanics responsible for asbestos clearance, unraveling the complexities of our body’s response to these potentially hazardous materials. By exploring the dynamic interplay between asbestos fiber characteristics and the lung’s defensive responses, we aim to provide a clearer understanding of how certain fibers may evade natural clearance, contributing to serious health implications.
Physiological Mechanics of Asbestos Clearance
Respiratory Repercussions: A Detailed Analysis of Pulmonary Responses to Asbestos Inhalation
In the realm of occupational health and respiratory physiology, the inhalation of asbestos fibers stands as a profoundly serious concern. To comprehend the pulmonic response to these minuscule, yet perilous, fibers, one must delve into the intricacies of both the structure of asbestos and the pathophysiological mechanisms it incites within the lungs.
Asbestos, once heralded for its durability and resistance to heat, comprises silicate minerals with a fibrous nature. These fibers, when disrupted, become airborne and susceptible to inhalation. Their diminutive size allows them to penetrate the pulmonary defenses and embed themselves deep within the lung tissue.
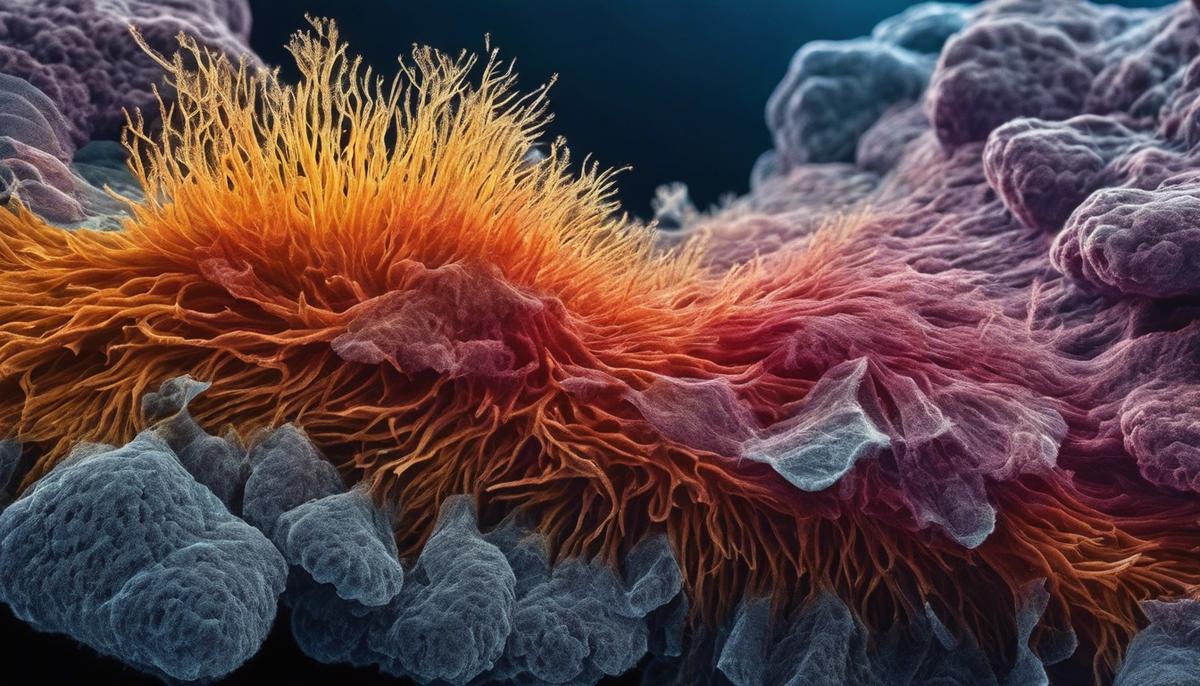
Upon entering the respiratory system, asbestos fibers confront the primary defense mechanism: the mucociliary escalator. This apparatus, consisting of mucus and cilia, typically entraps and expels foreign particles. Nevertheless, the sharp, needle-like form of asbestos fibers impedes this process, allowing them to journey farther into the recesses of lung tissue.
Once past these initial defenses, asbestos fibers lodge themselves within the delicate alveolar sacs—site of the vital gas exchange process. The body perceives these fibers as foreign invaders, eliciting an immune response. Macrophages, the phagocytic cells of the immune system, attempt to engulf and digest the fibers. But unlike organic pathogens, asbestos is inorganic and resistant to breakdown. The frustrated efforts of these immune cells culminate in an inflammatory response, which can cause cellular damage.
Persistent inflammation provoked by asbestos leads to a fibrotic reaction, where scar tissue or fibrosis forms within the pulmonary matrix. As a consequence, tissue elasticity wanes, translating to compromised lung function. Referred to as asbestosis, this condition is characterized by progressive dyspnea—labored breathing—which intensifies over time.
Further complication arises from the fact that inhaled asbestos fibers can also serve as a carcinogenic agent, promoting the development of malignancies such as mesothelioma, a rare and aggressive form of cancer affecting the pleural lining of the lungs.
The period between asbestos exposure and the manifestation of pulmonary issues can be significantly protracted, often spanning several decades. This latency challenges both diagnosis and causal attribution, complicating medical intervention.
In conclusion, the inhalation of asbestos fibers initiates complex pathways culminating in inflammation, fibrosis, and an increased risk of cancer, each contributing to the degradation of pulmonary function. The establishment of stringent regulatory measures to limit exposure to asbestos remains a critical step in safeguarding respiratory health in affected populations.
Health Impacts of Asbestos Accumulation
The health consequences of asbestos accumulation in the lungs extend beyond the initially visible symptomatic manifestations. As asbestos fibers accumulate, they pose an insidious risk given their resistance to biodegradation and their ability to persist in the pulmonary tissue for extended periods.
This resilience of asbestos fibers contributes to a chronic pathophysiological condition where the lung architecture becomes compromised. Over time, the elastic and spongy tissue of the lungs, critical for gas exchange, becomes increasingly scarred and rigid—a process known as fibrotic change. This scarring reduces lung capacity and elasticity, leading to compromised respiratory function.
The scarred tissue does not partake in gas exchange, which diminishes the lungs’ oxygenation capacity. Consequently, individuals may experience an ever-increasing difficulty in breathing, a condition known as progressive respiratory insufficiency. The decrease in lung function also leads to complications such as reduced exercise tolerance and, in advanced stages, may contribute to heart strain.
Another serious consequence is the heightened susceptibility to lung infections. As the lung’s structure and defense mechanisms degrade, the likelihood of contracting infections such as bronchitis or pneumonia escalates, each episode potentially exacerbating lung damage further.
The cumulative effects of these pathological changes precipitate a decline in the overall quality of life, with patients facing not only physical challenges but the psychological burden of chronic illness as well. Monitoring and managing lung health, therefore, becomes a lifelong commitment for those with significant asbestos exposure.
It’s worth noting that while asbestos-related lung conditions primarily concern respiratory function, the systemic implications of chronic lung disease should not be understated. Hypoxemia—low blood oxygen levels due to impaired lung function—can lead to far-reaching effects on multiple organ systems, including the brain and kidneys.
Moreover, the chronic inflammatory state induced by the presence of asbestos may also have putative links to systemic autoimmune conditions. However, the establishment of direct causality between the presence of asbestos fibers and autoimmune disease development necessitates further rigorous investigations.
Through continued examine, a comprehensive understanding of asbestos-related lung conditions can be ascertained. The cumulative knowledge aids in fostering informed decisions and advancements in public health policy, occupational safety, and treatment protocols.
As we move forward, it is imperative to continue prioritizing education and awareness to prevent asbestos exposure, thus safeguarding future generations from the lasting health consequences that have burdened the present.

Asbestos Fiber Characteristics
The salient characteristics of asbestos fibers that influence their retention or clearance from pulmonary structures form a critical facet of occupational health studies. Paramount among these attributes are fiber dimensions, which include both length and diameter, and the biopersistence, or the fiber’s resistance to physiological clearance mechanisms.
Asbestos fibers are categorized by their size; those exceeding 5 micrometers in length and having a diameter less than 3 micrometers are notably recalcitrant to clearance. Their slender, needle-like form allows them to penetrate deeply into the lung parenchyma, evading expulsion via the mucociliary escalator. Such dimensions also impede phagocytosis—the cellular engulfment process—rendering the fibers insusceptible to macrophage-mediated clearance. Conversely, shorter and thicker fibers tend to be more readily cleared from the respiratory system through mechanical and cellular processes.
The chemical composition of asbestos fibers contributes to their biopersistence. The body’s efforts to dissolve these amphibole or serpentine minerals are largely ineffective due to their high silicate content, leading to persistence within the pulmonary tissue. This inertness against biochemical breakdown facilitates the accumulation of fibers, thereby exacerbating tissue irritation and perpetuating inflammation.
Furthermore, the surface properties of asbestos, such as charge and reactivity, can potentiate lung retention. Fibers with higher surface reactivity can bind more tenaciously to tissues or cellular components, invoking sustained inflammatory responses.
These physicochemical characteristics consolide to render the clearance of asbestos fibers from the lungs a protracted process. The chronic nature of retention defines the trajectory of its pathogenic potential, a sobering truth underscoring the imperatives of exposure control and continuous research within this domain.

Exposure Assessment and Risk Management
Quantification of asbestos exposure and risk management are critical components in the endeavor to protect public health.
Asbestos exposure, particularly in occupational settings, is measured in fiber-years, which is a calculated metric that combines the concentration of fibers in the air (fiber per cubic centimeter) with the duration of exposure (years).
This quantification is crucial as the risk associated with asbestos exposure is dose-dependent; higher concentrations and longer durations increase the probability of adverse health effects.
Air monitoring is a primary method for quantifying asbestos exposure. Samples of ambient air are collected in environments where asbestos-containing materials are present or being disturbed, for instance during demolition or renovation of old buildings.
These samples are analyzed using phase-contrast microscopy (PCM) or transmission electron microscopy (TEM), with TEM allowing for more precise detection of asbestos fibers by distinguishing them from other fibrous materials.
Quantitative exposure assessment informs risk management strategies, which may include engineering controls, such as local exhaust ventilation to reduce fiber concentrations in the air; administrative controls, such as limiting the time workers spend in high-exposure environments; and personal protective equipment (PPE), including respirators and protective clothing.
These strategies aim to minimize inhalation of asbestos fibers, mitigating the potential for lung damage and disease development.
Risk management also encompasses medical surveillance for individuals with known exposure to asbestos. Regular health screenings, including chest radiographs and lung function tests, are paramount for the early detection of asbestos-related diseases.
Surveillance supports the timely initiation of medical interventions, potentially improving prognoses and extending lifespans for those affected.
Lastly, education and training are indispensable tools in asbestos risk management. Ensuring that workers and employers understand the hazards associated with asbestos, proper handling procedures, and emergency protocols is instrumental in minimizing exposure and safeguarding health.
Compliance with safety standards and regulatory frameworks is enforced through mandatory training sessions and the dissemination of guidelines provided by institutions such as the Occupational Safety and Health Administration (OSHA) and the Environmental Protection Agency (EPA).
As current and future studies shed more light on the intricacies of asbestos exposure and its health repercussions, continual refinement of risk assessment tools and management strategies is essential.
Only through persistent vigilance and scientific inquiry can the challenges posed by asbestos be addressed, ensuring a safer and healthier environment for all.

Advanced Asbestos Fiber Analysis
Modern scientific techniques have dramatically expanded our comprehension of the behavior of asbestos fibers within pulmonary structures. The advent of sophisticated imaging modalities, such as high-resolution computed tomography (HRCT), facilitates an unprecedented visualization of fibrous deposits and associated lung tissue pathology. HRCT scans grant us the capability to discern subtle differences in tissue density, enabling the identification of early fibrotic changes that might elude conventional radiography.
Further, bronchoalveolar lavage (BAL) provides a minimally invasive method to collect cells from the lower respiratory tract, offering a window into the cellular and molecular milieu influenced by asbestos fibers. Flow cytometry, applied to BAL fluid samples, allows scientists to quantify and analyse immune cells and inflammatory markers, highlighting the altered immune landscape that accompanies asbestos-induced lung disease.
The application of proteomics and genomics to asbestos research is relatively nascent but powerfully transformative in understanding the intricate biochemical and genetic pathways involved. Advanced proteomic techniques have the potential to unveil specific protein biomarkers associated with asbestos exposure, offering insights into molecular mechanisms leading to lung injury and malignant transformation. Similarly, genomic studies have uncovered mutations in key tumor suppressor genes that might predispose individuals to mesothelioma following asbestos exposure.
Additionally, advanced spectroscopic methods provide detailed information about the chemical nature of asbestos fibers lodged in lung tissue. Energy-dispersive X-ray analysis (EDXA) applied in conjunction with analytical electron microscopy, for example, uniquely identifies the elemental composition of fibers, contributing to the knowledge of how different asbestos types invoke diverse pathological responses.
Finally, lung tissue biobanks hold preserved lung tissues from affected individuals, providing invaluable resources that enable longitudinal and cross-sectional studies. By comparing tissue samples of varying degrees of disease progression, researchers can track the pathophysiological evolution of asbestos-related diseases.
In effect, these sophisticated modern techniques act as a multifaceted arsenal, equipping scientists with the tools to scrutinize the behaviors of asbestos fibers within the lungs from macroscopic to molecular levels. Beyond aiding in our basic understanding, they serve as essential adjuncts in the ongoing effort to refine therapeutic approaches, enhance diagnostic accuracy, and develop preventative strategies. Thus, scientific inquiry persists unabated, driven by the imperatives of preserving pulmonary health and mitigating the legacy of asbestos.

Future Research Directions
Emerging Research Endeavors in Asbestos-Related Lung Diseases
As progress marches forward in our understanding of asbestos and its deleterious effects on pulmonary health, future research endeavors must pivot towards innovative strategies that will not only improve patient outcomes but also expand our knowledge base on how to control or eradicate the disease process induced by asbestos fibers. Current scientific quests are increasingly focused on the molecular and cellular dynamics of asbestos-related diseases, intending to decipher the convoluted pathogenesis and to design more efficacious treatments.
Foremost among these initiatives is the concerted effort to understand genetic susceptibility and epigenetic alterations in the context of asbestos exposure. Studies are examining the variation in individual genetic makeup that may predispose some to graver health outcomes than others, even with similar exposure levels. Epigenetic research explores how environmental factors like asbestos can alter gene expression without changing the DNA sequence itself, providing insight into the mechanisms of disease progression.
Another critical area of study is the quest for early detection biomarkers. Discovering specific molecules or genetic changes that can reliably indicate the earliest stages of asbestos-related lung disease allows for earlier intervention, potentially halting the progression of the disease and improving prognosis. Biomarkers are also being sought to predict how aggressively a disease may evolve, offering a tailored approach to treatment.
In terms of therapeutic prospects, the aim is to develop targeted treatments that can either prevent the fibrotic process or mitigate its effects. Advanced research is delving into antifibrotic drugs, which seek to interfere with the biochemical pathways that lead to scarring in lung tissue. Gene therapy presents another promising frontier, aiming to repair or replace defective genes responsible for the body’s adverse response to asbestos fibers.
To complement these biological endeavors, there are likewise advances in imaging and detection technology. Innovations in imaging modalities are expected not only to aid in earlier diagnosis but also to assist in evaluating the efficacy of new treatments, thereby speeding up the drug development process. The adaptation and refinement of non-invasive techniques that can monitor disease progression in real-time are also anticipated.
The collective ambition of these initiatives is not solely the reduction of the burden of asbestos-related diseases but also the prevention of their occurrence. Public health strategies are being fine-tuned to incorporate recent findings into guidelines that can more effectively shield workers and the general population from harmful exposure. The synthesis of evidence from occupational health research, molecular biology, and clinical practice is paving a new era in the fight against one of the most challenging occupational hazards of the modern age.
Continued collaboration across disciplines and borders will undoubtedly be pivotal in the ongoing battle against asbestos-related lung diseases. Through such concerted efforts, it is hoped that the grim legacy of asbestos can be transformed into a narrative of triumph where science and humanity work hand in hand to protect and rehabilitate those who have suffered. The dedication to research, the commitment to eradicating disease, and the passion for improving public health stand as testaments to the resilience and tenacity inherent in the quest to conquer asbestos-related diseases.

Bridging the gap between exposure to asbestos and our body’s response is critical in protecting lung health and preventing the insidious diseases associated with this material. The collective efforts in advanced asbestos fiber analysis, exposure assessment, and risk management have made significant strides in understanding and mitigating these risks. Looking ahead, the focus on future research directions fosters hope for improved methods to augment lung clearance of asbestos and development of novel strategies to shield individuals from its harmful impact. As science continues to evolve, so does our capacity to safeguard our health from the invisible but tangible threats posed by lingering asbestos fibers in our environment.

