The silent penetration of asbestos fibers into the lungs remains one of the most insidious occupational hazards of the past century, with their impact on health manifesting stealthily over decades. Asbestos, a seemingly innocuous group of minerals, is renowned for its heat resistance and fibrous strength, traits that led to its proliferation in industries worldwide. This essay embarks on a crucial journey to unravel the complexities of asbestos inhalation, from the moment these microscopic fibers drift through the air until they lodge deep within the pulmonary landscape. By delving into the intricate dance of biology and mineralogy that occurs post-inhalation, we aim to shed light on the far-reaching consequences of asbestos exposure and the silent battle waged in the lungs of those affected.
The Nature of Asbestos and Inhalation
Title: The Inherent Hazards of Asbestos Inhalation
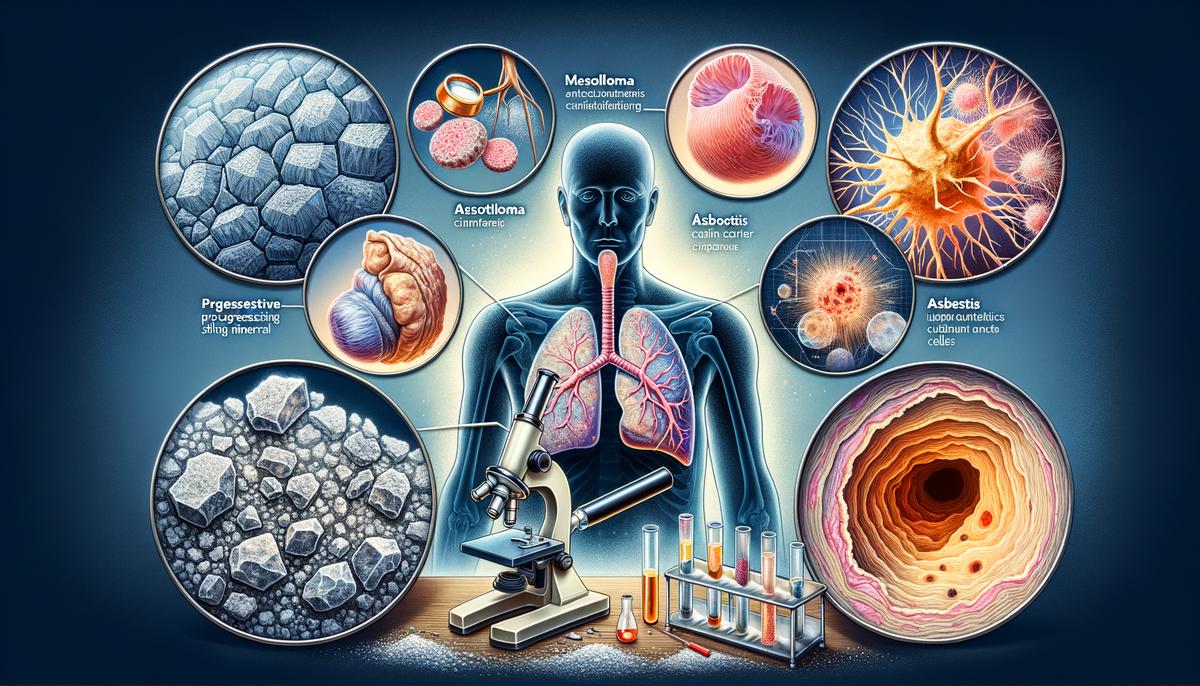
Asbestos, a term describing a set of six naturally occurring silicate minerals, has historically been praised for its desirable physical properties, including sound absorption, tensile strength, and resistance to fire, heat, and electrical damage. However, despite its utility across various industries, asbestos poses significant health risks when its fibers become airborne and are inhaled.
Upon inhalation, the unique properties of asbestos fibers contribute significantly to their hazardous nature. The microscopic fibrils that constitute asbestos can fracture into even finer fibers, less than a micrometer in width. Due to their minuscule size and aerodynamic shape, these fibers can be easily inhaled, bypassing the body’s natural respiratory filters such as nose hairs and the cilia within the bronchial tubes.
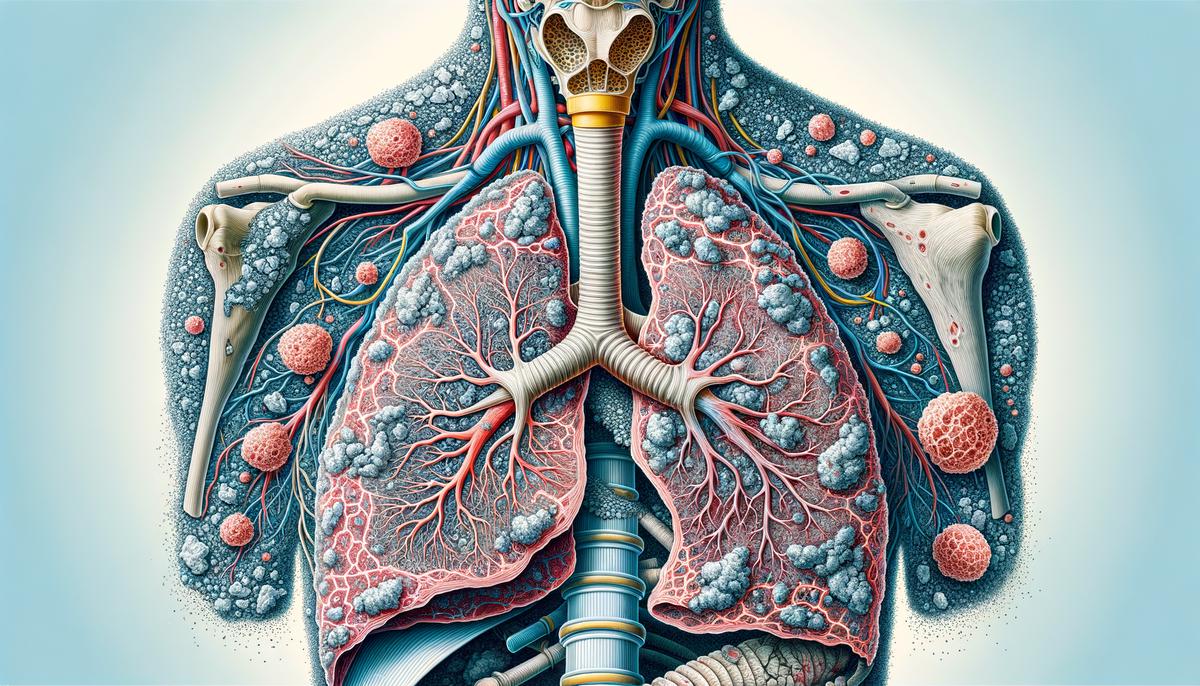
Once within the lung tissues, the properties that once made asbestos a highly sought-after building material become a liability to human health. The physical durability of asbestos, an asset in construction materials, means that it is biopersistent and can remain within lung tissue for extended periods, as the body is unable to break down or expel such robust fibers. These fibers can become lodged in the delicate alveolar sacs where oxygen exchange occurs, or in the mesothelium, the membrane lining the chest cavity.
Furthermore, asbestos fibers are not only physically intrusive but also chemically active. The needle-like shape of the fibers can puncture cellular and subcellular structures within the lung tissue, resulting in inflammation and cellular damage. This constant irritation increases the risk of cellular mutations, ultimately heightening the chances of lung diseases such as asbestosis, lung cancer, and mesothelioma, a lethal form of cancer specific to the mesothelium.
The health hazards of asbestos are compounded by the latency of asbestos-related diseases, often manifesting decades after initial exposure. This delayed onset makes it challenging to directly correlate exposure to the specific health outcomes until many years later, when the diseases have already progressed.
Overall, the rigorously studied and well-documented health consequences of asbestos inhalation arise from the inherent physical resilience and biological reactivity of asbestos fibers. These characteristics reinforce the necessity of stringent control measures to mitigate exposure and safeguard public health.

Pathophysiology of Asbestos in the Lungs
Upon entering the pulmonary system, asbestos fibers engage in a deleterious interaction with the tissue lining the respiratory tract and the alveoli, critical for the exchange of oxygen and carbon dioxide. Over time, the presence of these fibers initiates a chronic inflammatory response, as the body’s immune system endeavors to expel these foreign elements. Macrophages, immune cells designed to consume and neutralize invaders, ineffectively attempt to phagocytize the asbestos fibers due to their size and durability, leading to a continued inflammatory stimulus and the release of reactive oxygen and nitrogen species.
The cascade of inflammation and the release of these reactive molecules contribute to a series of alterations within the lung architecture. Fibroblasts, the cells responsible for the production and maintenance of connective tissue, are activated and proliferate. They deposit an excess of collagen and other extracellular matrix components, resulting in fibrosis, a scarring process that steadily diminishes pulmonary function. The elasticity and compliance of lung tissue are consequently reduced, leading to compromised respiratory mechanics. As fibrosis progresses, the airways and gas-exchange surfaces within the lungs are constricted and deformed, culminating in restrictive lung disease, characterized by reduced lung volumes and impaired gas exchange.
In addition to fibrosis, the mutagenic properties of asbestos also play an insidious role. The chronic exposure to asbestos fibers contributes to genetic and cellular mutations. These genetic damages, accumulated over time, have the potential to disrupt normal cell cycle control mechanisms, paving the way for neoplastic transformation which can manifest as lung cancer or mesothelioma.
Lastly, the pleura, a serous membrane wrapping the lungs, can be afflicted as well. With the extended presence of asbestos fibers within the pleural cavity, pleural plaques – calcified fibrotic areas – emerge, signaling the pathological remodeling of the pleura. Such alterations can evolve into pleural effusions or diffuse pleural thickening, further contributing to respiratory distress and dysfunction.
Monitoring and maintaining safe environments to prevent asbestos exposure remains paramount, as these physiological and pathological manifestations develop insidiously over protracted periods, often going unnoticed until they reach advanced stages, where interventions are notably less effective. Hence, understanding the progressive nature of these pathologies underscores not just the imperative for early detection and treatment, but also the critical need for stringent regulatory standards to prevent asbestos exposure and protect respiratory health.
Health Conditions Associated with Asbestos Exposure
Continuing from the comprehensive overview of the multifaceted hazards posed by asbestos, this discourse aims to elucidate the long-term health conditions springing from its exposure. It is imperative to acknowledge the considerable impact asbestos has on organs beyond the pulmonary system.
Over time, the presence of asbestos fibers can initiate a domino effect, potentially leading to diseases within the digestive system. For instance, prolonged asbestos exposure has been linked with an increased risk of gastrointestinal cancers, inclusive of colorectal and stomach cancer. The proposed mechanism involves the ingestion of asbestos fibers, which, like their respiratory counterparts, can embed themselves in the stomach and intestinal lining, thus precipitating a malignant transformation.
Additionally, asbestos exposure is correlated with immunological consequences; the immune system may be continuously stimulated to attack the persistent fibers, eventually leading to potential auto-immune responses or impairments in immunologic function. This can render an individual more susceptible to a range of illnesses and infections, thus diminishing overall health and resilience.
Within the cardiological context, asbestos exposure has been associated with increased risks of pericarditis and other cardiovascular diseases. It is hypothesized that chronic inflammation caused by asbestos can ultimately affect the heart, leading to heightened stress and potential damage to cardiac tissues.
Renal issues are also among the roster of long-term conditions associated with exposure. The National Institute for Occupational Safety and Health (NIOSH) has identified chronic kidney disease and renal cancers as potential risks for those with history of asbestos exposure. The precise biological processes underpinning these associations remain a subject of ongoing research.
It must be emphatically stated that these conditions manifest typically after decades of latency. Thus, individuals with even remote histories of asbestos contact should remain vigilant regarding their health. Moreover, the collective responsibility towards those affected by asbestos-related disorders cannot be overstated. Ensuring appropriate legislation, regulation, and remediation strategies is pivotal for the protection of public health.
In conclusion, asbestos presents a multitudinous array of long-term health repercussions. From pulmonary to immunological, from gastrointestinal to cardiovascular, and renal – the insidious nature of asbestos warrants persistent and collective efforts in surveillance and prevention. Acknowledging the spectrum of potential asbestos-induced pathologies underscores the extant need for continued research, rigorous risk management, and empathetic patient care.
Survival Rates and Prognostic Factors
Survival Rates and Prognostic Factors in Asbestos-Related Diseases
Asbestos-related diseases are notorious for their delayed presentation and challenging prognosis. Understanding the survival rates and factors influencing the prognosis is paramount for healthcare providers and patients alike.
Survival rates for asbestos-related diseases vary significantly based on the type and stage of the disease at diagnosis. Among these conditions, mesothelioma – a rare and aggressive cancer caused by asbestos exposure – has notably low survival rates, with most studies indicating a median survival of one to two years after diagnosis. Lung cancer associated with asbestos exposure also has a poor prognosis, with five-year survival rates ranging from 15% to 30%, depending on the stage at which the cancer is diagnosed.
Prognosis for individuals with asbestos-induced lung diseases is contingent upon several pivotal factors, including the type and extent of asbestos exposure, the latency period of the disease, the age and overall health of the individual at the time of diagnosis, and the presence of other health conditions, such as smoking-related diseases. Furthermore, early detection plays a crucial role in determining the course of the disease; therefore, individuals with known asbestos exposure must be vigilant about regular health screenings.
The effectiveness of therapeutic interventions significantly influences survival rates. Treatment options and their efficacy can vary, with protocols including surgery, chemotherapy, and radiation therapy. The multidisciplinary approach, where specialists collaborate to tailor treatment to the individual’s specific condition, can improve survival times and quality of life.
Occupational histories are key in making a prompt diagnosis, as they can guide clinicians to suspect and screen for asbestos-related diseases, particularly in patients presenting with respiratory symptoms and a history of exposure. Notably, prognosis is generally more favorable for diseases such as asbestosis if caught in early stages. Asbestosis, a pulmonary fibrosis caused by asbestos exposure, has a variable prognosis that largely depends on the cessation of exposure and the prevention of further lung damage.
Survival rates of individuals with asbestos-related diseases are influenced by genetics as well, with research indicating that certain genetic profiles may confer susceptibility or resistance to developing these conditions. Additionally, psychosocial factors, such as access to healthcare and support systems, can impact patient outcomes.
To conclude, the prognosis for asbestos-related diseases is influenced by a multitude of factors including disease type and stage at the time of diagnosis, patient characteristics, efficacy of treatment, occupational history, genetic factors, and psychosocial support systems. Continuous progress in medical research and treatment methodologies promises to enhance the survival rates and health outcomes for those afflicted by these severe conditions. Providers must maintain a high index of suspicion and advocate for regular health screenings in at-risk populations to facilitate timely intervention and optimal management of asbestos-related diseases.

Occupational and Environmental Asbestos Exposure
Asbestos lung retention and the perpetual danger it presents are of significant concern in occupational and environmental health. It is imperative to elucidate the mechanisms facilitative of the lingering presence of asbestos fibers within pulmonary structures subsequent to exposure. Alongside well-known asbestos-induced diseases, the long-term residence of asbestos in the lungs is also intricately connected with occupational and environmental exposures.
Occupational exposure to asbestos predominantly occurs in industries such as construction, mining, shipbuilding, and manufacturing of asbestos-containing materials. Workers are often in environments that are rife with asbestos dust, which easily becomes airborne. These fibers are then inadvertently inhaled during daily work responsibilities. Regulatory measures such as personal protective equipment, air monitoring, and safety protocols are vital in reducing this risk, yet despite adherence to safety guidelines, residual exposure can persist, augmenting the risk of fiber deposition in the lung tissue.
Environmental exposure, on the other hand, often results from the degradation or disturbance of asbestos-containing materials in older buildings or products. Natural disasters such as earthquakes and hurricanes can unleash asbestos fibers into the air, which can be inhaled by individuals in the affected vicinities. In addition, individuals living near asbestos mines or waste sites may be unknowingly subjected to chronic, low-level environmental exposure. Legislation aimed at the safe removal, disposal, and management of asbestos is crucial in mitigating these environmental risks.
Once embedded in the lung tissue, asbestos fibers can remain lodged due to their morphological characteristics—long, thin, and durable. Their size allows them to penetrate deep into the lungs, while their physical resilience makes them resistant to breakdown and expulsion. This, combined with the fibers’ tendency to evade the natural clearance mechanisms of the lungs, includes the mucociliary escalator and macrophagic activity, meaning that these fibers can persist for extended periods.
The long-term presence of asbestos in the lungs is also exacerbated by repeated exposures. In occupational settings, workers may be exposed on a day-to-day basis for years, leading to a cumulative effect. While certain job sites may endeavour to implement best practices, the historical use of asbestos means that legacy exposure risks continue to plague certain professions.
Furthermore, the capacity of asbestos fibers to incite chronic pulmonary inflammation and scarring (fibrosis) contributes to their persistence. The inflammatory milieu can encourage the production of fibrous tissue that may encapsulate the fibers, sequestering them further within pulmonary architecture.
In light of these concerns, it is incumbent upon industrial hygienists, researchers, and policy-makers to intensify their commitments to prevent exposure, enhance diagnostic acumen, and advance treatment modalities. This concerted effort would not only mitigate new instances of exposure but also provide support for those with extant lung retention of asbestos fibers. Continuous advancements in asbestos detection and removal technologies are also paramount to decrease environmental and occupational exposure to asbestos.
With a deeper understanding of the factors contributing to the retention of asbestos fibers in the lungs, emphasis can be placed on the implementation of measures that minimize exposure and the burden of asbestos-related diseases on workers and the general public alike.

Advancements in Research and Treatment
Diagnosis and treatment of asbestos-related lung conditions necessitate a multi-faceted approach, taking into account the indolent nature of these diseases and the complexity of the underlying pathophysiological mechanisms. The latest research in this domain encompasses novel diagnostic tools, therapeutic strategies, and a better understanding of disease prognosis which is vital for improving patient outcomes.
Advanced Diagnostic Techniques:
The advent of sophisticated imaging technologies such as High-Resolution Computed Tomography (HRCT) has significantly enhanced the ability to detect asbestos-related abnormalities in lung tissue with greater precision. Moreover, researchers are exploring the utility of biomarkers—proteins or other molecules in body fluids—that can indicate the presence of asbestos-related diseases even before symptoms are manifest. Identifying such biomarkers could revolutionize early detection and intervention, potentially altering the disease course.
Medical Therapeutic Strategies:
Asbestos-related lung diseases have traditionally been resistant to treatment, but burgeoning methodologies have exhibited promise. For mesothelioma, immunotherapy—a type of treatment that uses the body’s immune system to recognize and attack cancer cells—has emerged as a powerful adjunct to standard chemotherapy regimens. Additionally, targeted therapies that isolate specific genetic mutations or cell pathways involved in cancer proliferation are under investigation in clinical trials.
Gene therapy is another area of exploration, where researchers intend to repair or replace mutated genes in the lungs to stop the progression of cancer. While still in early stages, this avenue of research holds substantial potential for future applications.
Pulmonary Rehabilitation:
For individuals suffering from decreased lung function due to diseases like asbestosis, pulmonary rehabilitation programs aim to improve quality of life through customized exercise and education plans. These interdisciplinary programs address physical, psychological, and social implications of lung diseases, facilitating a better lifestyle for affected individuals.
Preventive Measures and Supportive Care:
Ongoing efforts in research also focus on improving preventive and supportive care measures. The implementation of rigid work safety regulations and improved environmental monitoring have been crucial in reducing the incidence of asbestos exposure. Simultaneously, palliative care principles are increasingly integrated into treatment protocols to relieve symptoms, reduce suffering and support the psychological well-being of patients with advanced diseases.
Technological Innovation:
Nanotechnology has the potential to revolutionize the field with the development of novel drug delivery systems to target lung tissues specifically affected by asbestos fibers. Researchers are also investigating the use of robots and other advanced techniques for the safe removal and disposal of asbestos materials from buildings, thereby reducing the risk of exposure to occupational workers and the environment.
In conclusion, the battle against asbestos-related lung conditions is fought on a broad front encompassing prevention, early detection, robust treatment, and palliative care. Each stride in research and clinical practice arms healthcare professionals with better tools to manage these complex diseases, offering hope for improved patient outcomes and a future where the impact of asbestos-induced diseases might become substantially diminished.
Through the layers of information and narrative, we have journeyed from the dusty factories and construction sites to the inner sanctum of the human respiratory system, witnessing the profound impact of microscopic fibers on human health. Our exploration has spanned the cellular reactions to the global efforts aimed at combatting this lingering health menace. Armed with the knowledge of the perils of asbestos and the resilience of the human spirit, we witness the ongoing evolution of safety practices, medical advancements, and scientific pursuits. It is in the confluence of these elements that hope takes root, fostering a future where the tale of asbestos in the lungs is one of historical reflection rather than current fear.

