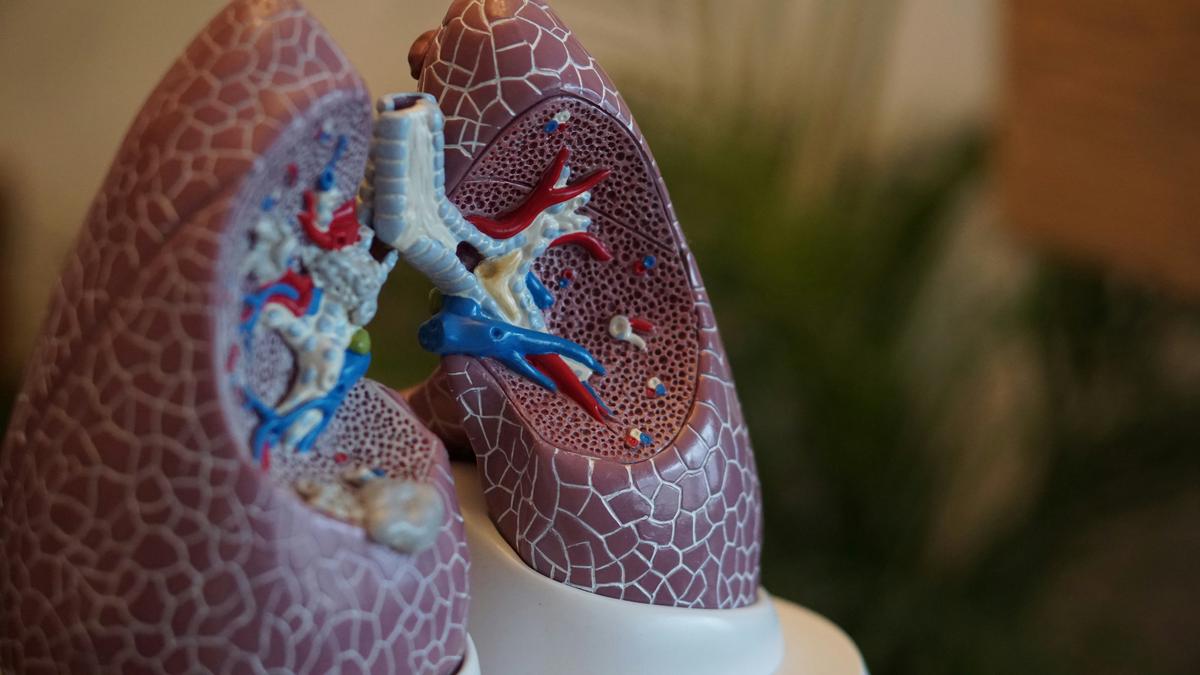
The mere utterance of ‘asbestos’ can evoke a sense of trepidation due to its infamous association with a host of serious health complications affecting the lungs. This ubiquitous yet perilous mineral, once praised for its fire-retardant properties, now stands as a somber testament to occupational and environmental health risks. Our exploration into the realm of asbestos-related lung disease embarks with a deep dive into the pathophysiology behind this insidious threat. Understanding how asbestos fibers infiltrate lung tissue, spark inflammation, and incite fibrotic changes is pivotal to unraveling the enigma of asbestos-induced pathologies, including asbestosis, lung cancer, and mesothelioma. Armed with the latest peer-reviewed research, we endeavor to piece together the puzzle of how these minuscule fibers wreak havoc on a microscopic scale, leading to life-altering pulmonary conditions.
Pathophysiology of Asbestos-Related Lung Disease
Title: Unraveling the Nexus Between Asbestos Exposure and Respiratory Diseases
Asbestos, a term that encapsulates a group of naturally occurring fibrous minerals, is notorious for its insidious impacts on human health. Historically lauded for its heat resistance, tensile strength, and insulating properties, it has been deployed extensively across various industries until its dark side was irrefutably exposed. Whilst the utilitarian benefits of asbestos are manifold, its injurious effects on respiratory health are particularly harrowing and merit a closer examination.
Upon inhalation, asbestos fibers, due to their diminutive and aerodynamic nature, circumnavigate the body’s natural defenses and lodge themselves in the depths of the lung tissue. These fibers are particularly obstinate; once settled in the pulmonary system, they resist breakdown by the body’s immune mechanisms. The persistent presence of these fibers can invoke a chronic inflammatory response in which the body relentlessly attempts to expunge these indigestible intruders, to no avail. This inflammation is the preamble to a cascade of deleterious health effects that may ensue.
Asbestosis, a form of pulmonary fibrosis, emerges as a direct consequence of asbestos exposure. It is characterized by the scarring of lung tissue that progressively impedes the capacity of the lungs to expand and contract. This scarring throttles the efficient exchange of gases, leading to compromised oxygen intake and the retention of carbon dioxide. Sufferers may experience symptoms such as persistent coughing, chest tightness, and dyspnea – a labored breath that can escalate into a pronounced disability.
Moreover, asbestos exposure is inextricably linked to malignant respiratory conditions such as lung cancer and mesothelioma. Mesothelioma, a particularly virulent form of cancer, targets the mesothelial cells lining the lungs, chest, abdomen, and heart. Its relationship with asbestos is so strong that the majority of mesothelioma cases are directly attributable to asbestos exposure. The pathology of these cancerous afflictions is complex. The fibers engender mutation-inducing DNA damage in cells, which, compounded by the chronic inflammatory state, propels the evolution of malignancy.
Respiratory diseases induced by asbestos are insidious in nature; they often lie dormant for years, the latency period spanning decades. Recognition and diagnosis of asbestos-related illnesses hinge upon a confluence of patient exposure history, clinical evaluation, and radiological assessment. Preemptive measures entail strict adherence to safety protocols and regulations concerning the handling of asbestos, as well as rigorous abatement procedures to curtail the release of fibers in environments where asbestos is present.
In conclusion, asbestos embodies a significant occupational and environmental hazard. Knowledge and understanding of its destructive potential on respiratory health have burgeoned over the years, underscoring the imperative for stringent control measures not only to protect individuals but also to preserve the sanctity of public health.

Diagnostic Procedures for Asbestos-Related Conditions
Current best practices in the diagnosis of asbestos-induced respiratory issues revolve around a combination of detailed patient history, radiological imaging, and, where necessary, pathologic examination of lung tissue.
The initial approach involves a comprehensive review of the patient’s occupational history, particularly focusing on any known exposure to asbestos. It is vital to document the duration and intensity of exposure, as these factors are directly related to the risk of developing asbestos-induced respiratory issues. Non-occupational exposures, such as living in close proximity to asbestos mines or using asbestos-containing products, should also be considered.
Radiographic techniques are pivotal in the evaluation of suspected asbestos-related diseases. Chest radiography remains a useful tool in identifying pleural thickening and lung fibrosis, whilst High-Resolution Computed Tomography (HRCT) is superior for detecting early changes, such as lung nodules or the distinctive ‘honeycomb’ lung pattern associated with asbestosis. HRCT is also essential in evaluating the pleura, where plaques may be indicative of past asbestos exposure.
Pulmonary function tests (PFTs) assess the impact of the disease on lung function, often revealing a restrictive pattern in asbestos-related respiratory illnesses. Importantly, PFT results help in the evaluation of disease severity and could influence treatment decisions.
For cases where diagnosis remains uncertain after non-invasive methods, invasive procedures may be employed. Bronchoscopy with bronchoalveolar lavage (BAL) can collect cells from the lung for analysis, sometimes showing higher levels of certain types of cells, which can be suggestive of asbestos exposure. Furthermore, thoracoscopy or video-assisted thoracic surgery (VATS) allows for direct inspection of the pleura and collection of larger biopsy samples, essential in confirming mesothelioma.
Biomarkers are an emerging domain, with research suggesting that certain soluble mesothelin-related peptides in the blood may serve as indicators of mesothelioma. However, the use of biomarkers is not yet standardized and should currently be considered adjunctive to other diagnostic methods.
A multidisciplinary approach is recommended, involving pulmonologists, radiologists, and pathologists, to ensure an accurate diagnosis, guiding appropriate management and therapeutic interventions.
Regular follow-up of individuals with a history of asbestos exposure is crucial, not only for the early detection of asbestos-related conditions but also for monitoring the progression of disease in those already diagnosed.
The profound understanding of asbestos-induced respiratory issues necessitates a commitment to best practices which facilitate timely and accurate diagnoses. As advancements in diagnostic technology and methodology continue, it is the responsibility of the medical community to remain at the forefront of research, incorporating new evidence into practice, thereby improving outcomes for those affected by these serious conditions.

Treatment and Management of Asbestosis and Mesothelioma
Advancements in Treatment Strategies for Asbestos-Related Lung Diseases
Asbestos-related lung diseases represent a persistent and challenging public health concern. Due to the difficulty inherent in the eradication of existing asbestos and the latency of disease presentation, medical research has been continually advancing in the development of therapeutic strategies to combat the adverse health effects associated with asbestos.
The cornerstone of managing asbestos-related diseases lies predominantly in symptom management and supportive care. Supplemental oxygen, pulmonary rehabilitation, and medications to thin secretions are typical interventions for patients suffering from asbestosis, where the emphasis is on improving quality of life and functional status.
Pharmacologically, the focus is on mitigating the chronic inflammatory response inflicted by asbestos fibers. Corticosteroids are sometimes employed, although their efficacy is the subject of ongoing debate within the medical community. More promising are recent studies examining the role of antioxidants and anti-fibrotic drugs, which aim to reduce oxidative stress and fibrosis in the lung tissue, potentially slowing disease progression.
For lung cancer resultant from asbestos exposure, treatment aligns largely with standard oncological protocols, including surgery, chemotherapy, and/or radiotherapy, according to the stage and type of lung cancer present. Advances in target-specific drugs and immunotherapies have also started to find their place in treatment regimens, offering hope for improved outcomes.
Mesothelioma, the malignancy with a notably strong connection to asbestos exposure, has seen promising developments. The use of multimodal therapy, combining surgery with chemotherapy and/or radiation, offers the current best approach for eligible patients. Experimental therapies such as photodynamic therapy, gene therapy, and immunotherapy are under investigation and showing potential.
Moreover, clinical trials continue to be fundamental in the search for an effective cure, specifically for mesothelioma. Recent studies focus on checkpoint inhibitors and vaccines that trigger the immune system to recognize and attack cancer cells, providing an innovative direction in the arsenal against this formidable disease.
As one delves into the world of established and emerging therapies for asbestos-related lung diseases, it is clear that while much progress has been made, the path forward is marred by complexity. Thus, commitment to ongoing research, funding, and international collaboration remain imperative.
Continual advancements in molecular biology and pharmacology bear the promise of more targeted and effective treatments. Looking ahead, it is the collaborative effort between healthcare providers, patients, researchers, and policy makers that will ultimately pave the way towards substantive breakthroughs offering renewed hope for those affected by the indelible impact of asbestos exposure.
Prevention and Public Health Strategies
To further elucidate upon the prevention of asbestos exposure and the diminution of its associated health risks, the approach must include a multifaceted strategy. At the cornerstone lies comprehensive regulation and legislation. Stringent occupational safety standards, augmented by robust enforcement mechanisms, are vital elements in impeding asbestos exposure. These standards ensure that proper protective equipment, such as respirators and protective clothing, are standardized and available for those at risk. Moreover, rigorous training for workers dealing with asbestos is indispensable to diminish inadvertent exposure. It is crucial that this instruction encompasses the correct usage of protective gear, safe handling practices, and immediate procedures in the event of accidental exposure.
Proactive asbestos surveillance and abatement programs are paramount in identifying environments at risk. It is essential that buildings, especially older structures, undergo routine inspections to ascertain the presence of asbestos-containing materials. Should these materials be detected, deliberate management or removal plans must be executed, adhering to stringent safety protocols to prevent fiber release into the air. Moreover, these abatement efforts should be overseen by certified professionals to minimize the risk of propagation of fibers during the process.
Public health initiatives are also vital components in mitigating asbestos exposure and its consequences. Educational campaigns can significantly elevate awareness regarding asbestos risks, safe removal practices, and the importance of early detection of asbestos-related diseases. These campaigns can extend their reach not only to workers in industries with historical asbestos exposure, but also to residents living in proximity to contaminated sites, and to the general population, fostering an informed society cognizant of asbestos implications.
Healthcare professionals are also integral to preventing asbestos-related disease. By engaging in continuous medical education, physicians can sharpen their acumen for recognizing symptoms and the nuanced presentations of asbestos-related illnesses. Early detection can influence treatment outcomes positively; thus, awareness and knowledge become powerful tools in the physician’s repertoire.
Finally, an indirect yet profound measure in averting asbestos-related health issues is the innovation and adoption of alternative materials. By investing in research and popularization of safe substitutes, public dependency on asbestos can diminish considerably. The cessation of asbestos usage and its replacement with non-hazardous alternatives will undeniably be instrumental in decreasing exposure instances and subsequent health repercussions.
To encapsulate, the overarching strategy to prevent asbestos exposure and curtail its public health impact necessitates an amalgamation of regulatory actions, education, professional training, and continued advancement in safer alternatives. Together, efficacious implementation of these measures heralds improved outcomes in the protection and health of both workers and the general public against the unseen yet significant threat posed by asbestos.

Embarking on the quest to mitigate the impact of asbestos on human health, we have traversed the landscape of pathophysiology, diagnostic intricacies, treatment avenues, and preventative measures. The interconnected tapestry of clinical practices and public health initiatives stands as our collective armamentarium against this environmental adversary. As we marshal onward, it is the continual synthesis of advanced diagnostics, innovative treatments, and robust prevention strategies that illumines the path toward safeguarding our respiratory health. While the specter of asbestos-related diseases looms, it is through concerted efforts encompassing regulation, education, and unwavering vigilance that we can aspire to a future where the air we breathe is untainted by the shadows of the past.

