Asbestos, once hailed as a miracle mineral due to its heat resistance and durability, has since become synonymous with serious health implications when inhaled. At a molecular level, the fine, fibrous structure of asbestos presents a perilous risk; if disturbed, the fibers can embed themselves in lung tissue, leading to a cascade of pathophysiological effects. The focus of this discourse is on unraveling the complexities of asbestos exposure, scrutinizing the mechanisms through which these seemingly innocuous fibers precipitate chronic inflammation, cellular atypia, and an increased propensity for cancerous growths, such as mesothelioma and lung cancer. Beyond the cellular battleground, our attention pivots to the diagnostic frontiers, exploring the most innovative techniques that enable early detection of asbestos-related diseases—a pivotal step towards a more favorable prognosis.
Pathophysiology of Asbestos Exposure
Title: The Cellular Impact of Asbestos on Human Physiology
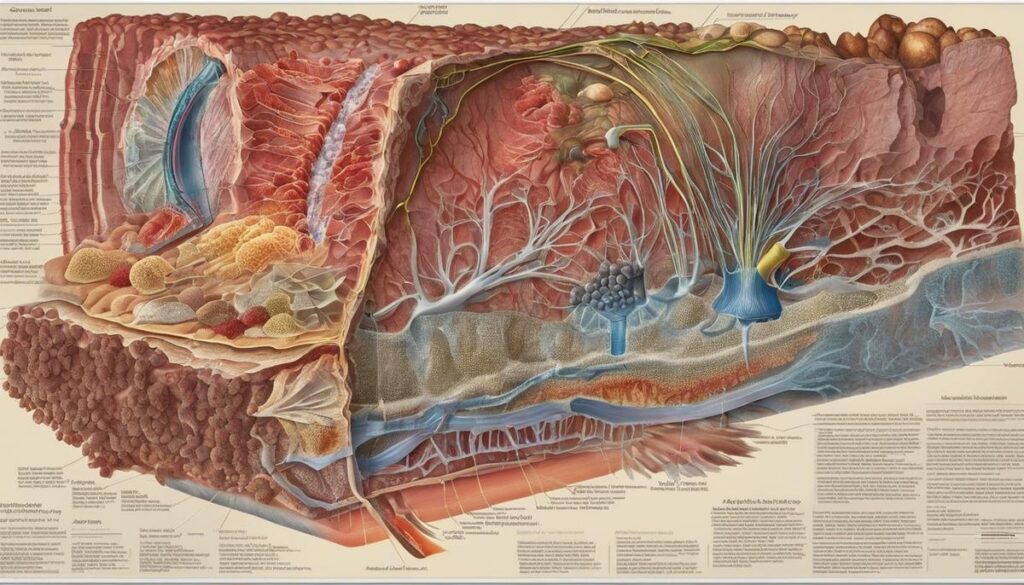
Asbestos, a group of naturally occurring fibrous minerals, once hailed for its versatility, has been incontrovertibly linked to detrimental effects on human health. Upon inhalation, these microscopic fibers navigate the intricate labyrinth of our respiratory system, ultimately embedding themselves within the delicate tissues of our lungs and, over time, inducing a cascade of cellular disruptions.
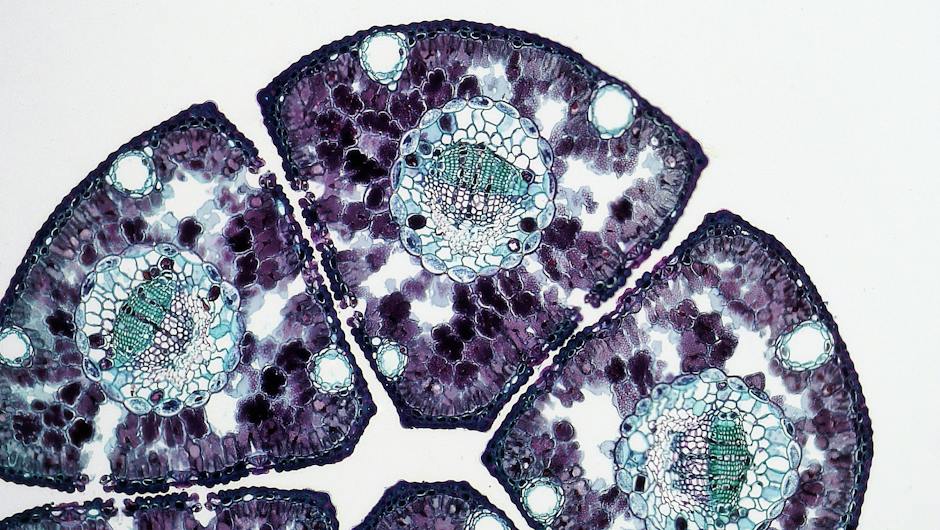
The pathogenesis begins when asbestos fibers elude the body’s primary defenses and reach the alveoli—the minute air sacs in the lungs where gas exchange occurs. Macrophages, a type of immune cell, attempt to phagocytize, or engulf, these fibers to eliminate them. However, due to the fibers’ size and resistance to breakdown, the macrophages are unable to digest them completely. This futile process results in the release of inflammatory mediators and reactive oxygen species, which are molecules known to cause damage to cellular structures.
These inflammatory signals have a two-fold effect. Firstly, they recruit additional immune cells to the site, perpetuating the cycle of inflammation. Secondly, they can cause direct injury to the cellular DNA within the mesothelial cells lining the lungs and the pleura, the membrane enveloping the lungs. This DNA damage is a pivotal precursor to the mutations that can lead to mesothelioma, a cancer attributed almost exclusively to asbestos exposure.
Another deleterious outcome arises from the interaction of asbestos fibers with lung tissue cells. The chronic irritation perpetuates a scarring process known as fibrosis. The accumulation of fibrotic tissue impedes normal lung function, leading to a condition known as asbestosis. This condition is characterized by a progressive decline in lung capacity, culminating in compromised respiration and oxygen diffusion.
It is also essential to recognize that asbestos has broader systemic effects beyond the pulmonary system. The fibers may migrate, or become translocated, to other areas of the body, potentially instigating similar pathological processes in different organs and tissues.
The intrinsic properties of asbestos fibers and their unique interactions with human cellular and immune systems elucidate the peril they pose to human health. Understanding the cellular impact of asbestos is paramount to developing effective diagnostic, therapeutic, and preventive measures against the diseases it may cause. The knowledge garnered from rigorous scientific research underscores the need for continued vigilance and regulatory measures to protect human health from asbestos exposure.
Diagnostic Methods for Asbestos-Related Diseases
Asbestos-related diseases present a formidable challenge to the medical profession both in terms of a diagnosis and treatment. The latency period between exposure and onset of symptoms can span decades, which necessitates a thorough and multifaceted approach to diagnosis. Here, the current diagnostic tools and criteria for asbestos-related diseases will be elucidated to foster a deeper understanding of these complex conditions.
Imaging studies constitute the first line of diagnostic tools in the identification of asbestos-related diseases. Chest radiography (X-rays) often reveals irregularities in lung tissue, such as thickened pleura and calcifications that suggest past asbestos exposure. However, high-resolution computed tomography (CT) scans provide greater detail and are superior in detecting interstitial lung diseases, including asbestosis, at an earlier stage than traditional X-rays.
Pulmonary function tests (PFTs) are crucial in quantifying lung function impairment that results from asbestos-induced lung disease. These noninvasive tests measure lung volume, capacity, and gas exchange to assess the presence and severity of restrictive lung diseases such as asbestosis.
When mesothelioma is suspected, tissue biopsy remains the gold standard for diagnosis. Various techniques including thoracoscopy, bronchoscopy, and fine needle aspiration are employed to obtain tissue samples from affected areas. Pathological examination of these samples is then performed to detect characteristic changes and confirm the presence of mesothelioma cells.
The definitive diagnosis of asbestos-related diseases involves correlating clinical findings with a thorough patient history of asbestos exposure. Occupational histories are reviewed to gauge the likelihood of exposure, with consideration given to both the duration and intensity of exposure events.
Furthermore, the criteria for diagnosing asbestos-related diseases have been refined over the years. For asbestosis, the American Thoracic Society has established guidelines that involve documented history of asbestos exposure, radiographic evidence or CT scan findings consistent with asbestosis, and pulmonary function test that indicate restrictive patterns.
In recent studies, biomarkers have also been explored as diagnostic tools. Certain serum and pleural biomarkers can suggest the presence of mesothelioma or other asbestos-related diseases; however, their utility in clinical practice requires further research before they can be employed as routine diagnostic measures.
Finally, the evolution of these diagnostic tools and criteria is ongoing. Research continues to unveil new methods and refine existing ones, enhancing the accuracy with which these diseases can be detected and treated. The medical community constantly aims to improve methodologies, not only for diagnosis but also to facilitate better patient outcomes and develop preventive strategies against asbestos-induced pathologies.

Current Therapeutic Interventions
Asbestos exposure has given rise to a variety of health conditions that require diligent medical intervention. Currently available treatment modalities focus on alleviating symptoms, slowing disease progression, and improving patients’ quality of life, as there is no cure for asbestos-related diseases. It is critical to address these modalities with seriousness due to their impact on numerous patients globally.
Firstly, a multi-disciplinary team approach is essential in managing asbestos-related conditions. Pulmonologists, oncologists, thoracic surgeons, radiologists, and other specialists often work collaboratively to tailor treatment plans to individual patient needs.
Regarding treatment for asbestosis, the scarring of lung tissue caused by prolonged asbestos exposure, management is predominantly supportive. Pulmonary rehabilitation is a cornerstone of treatment, aimed at enhancing lung function and capacity through therapeutic exercises and patient education. Inhalers, such as bronchodilators, may be prescribed to alleviate breathlessness by relaxing and opening the airways.
Oxygen therapy may be required in advanced stages of asbestosis to alleviate hypoxemia, a condition marked by low levels of oxygen in the blood. This intervention can significantly improve daily life and activity levels for afflicted individuals.
For those with malignant mesothelioma, treatment options are more varied and can include surgery, chemotherapy, radiation therapy, or a combination of these methods, known colloquially as multimodal therapy. Surgery aims to remove cancerous tissues; however, this option is contingent upon the stage of the disease and the overall health of the patient. Chemotherapy uses cytotoxic drugs to kill cancer cells or inhibit their growth and is often used when complete surgical resection of the tumor is not feasible. Radiation therapy can help control tumor growth and alleviate pain but is not typically curative for mesothelioma.
Emergent treatments such as immunotherapy, which leverages the body’s immune system to target and kill cancer cells, are under clinical trials and showing promise for mesothelioma. Targeted therapy that focuses on specific genetic mutations in tumor cells is another avenue being explored.
For other asbestos-related cancers, such as lung cancer, treatments mirror those of non-asbestos-related cancers of the same type and may include surgery, chemotherapy, radiation therapy, and targeted therapy based on the specific characteristics of the cancer.
Symptomatic treatments also play a critical role in the management of these conditions. Pain control may involve various analgesics, including nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and adjunctive medications like antidepressants or anticonvulsants, which can help control neuropathic pain. Palliative care, provided by a team specialized in offering physical, emotional, and spiritual support, is invaluable, particularly for patients with advanced disease.
As research advances, new treatment modalities are expected to emerge, evolving from a deepening understanding of the pathophysiology of asbestos-related diseases. Participation in clinical trials is encouraged when applicable, fostering access to novel therapies that may offer hope for improved outcomes. The healthcare community remains committed to exploring these innovative options, all in the endeavor to mitigate the deleterious effects wrought by exposure to asbestos.
In conclusion, the comprehensive approach to treating conditions caused by asbestos exposure requires a synergistic and evolving protocol that addresses the physical, emotional, and social aspects of these severe illnesses. While the treatment landscape continues to advance incrementally, the overarching goal remains steadfast: to afford those afflicted with the best possible care and prospects for a dignified life.

Photo by enginakyurt on Unsplash
Emerging Treatments and Research
Current Advancements in Asbestos-Related Disease Therapy: A Glimpse into the Future
As we progress into the future of medical science, the treatment of diseases resulting from asbestos exposure is entering a dynamic and arguably revolutionary phase. These developments encompass both the refinement of existing therapies and the exploration of groundbreaking treatments that offer hope for improved patient outcomes.
In recent years, a significant focus has been placed on targeted medical interventions. These interventions strive to pinpoint and disrupt molecular pathways critical to the progression of asbestos-related diseases. One such approach involves gene therapy, which aims to correct or mitigate the genetic alterations induced by asbestos fibers. Research indicates that modifying certain genes may inhibit tumor growth or enhance the immune system’s ability to combat malignancies like mesothelioma.
Additionally, there is a surge in the study of drugs that selectively interfere with specific cellular signals unique to asbestos-induced tumors. Known as signal transduction inhibitors, these drugs have the potential to halt tumor progression by blocking the transmission of growth signals within cancer cells.
Another avenue of research concerns the role of angiogenesis inhibitors. These drugs obstruct the formation of new blood vessels that tumors require for growth and survival. By cutting off the supply of nutrients and oxygen, these inhibitors can effectively starve tumors, potentially leading to their regression.
Furthermore, immunotherapy continues to gain traction as an emergent treatment modality. By harnessing and enhancing the body’s immune response, scientists aim to develop therapeutic vaccines that stimulate an immune attack specifically on cancer cells related to asbestos exposure. This method seeks to improve the specificity and efficacy of cancer treatments while minimizing adverse effects on healthy tissues.
In parallel, advancements in nanotechnology present a unique frontier in asbestos-induced disease therapy. Nanoparticles, due to their minute size, might deliver anti-cancer drugs directly to the site of the tumor, potentially increasing the concentration of the medication in the target area while reducing systemic side effects. Research into the application of such nanodrug delivery systems is underway, with the promise of enhancing the solubility and stability of chemotherapeutics.
Lastly, the concept of personalized medicine is increasingly influencing the approach to treating asbestos-related conditions. By analyzing the genetic and molecular profile of each patient’s tumor, clinicians aspire to tailor treatments that are the most effective for the individual. This method, although still in its nascent stages, stands to transform the current one-size-fits-all approach to a more sophisticated and personal strategy.
These emergent therapies and ongoing research endeavors represent the frontier of scientific efforts to mitigate and ultimately overcome the health challenges posed by asbestos exposure. Despite the complexity of this mission, relentless exploration, innovation, and unwavering commitment endure as the guiding lights in the field. As scientists and clinicians deepen their understanding of the disease mechanisms and treatment responses, there rests an unyielding hope for those touched by asbestos-related conditions and a world aspiring for their cure.

Prevention and Risk Management
Moving forward, the prevention of future asbestos exposure and the attendant health complications hinges on the consistent and rigorous application of safety measures and public health policies.
The encompassing strategy necessitates a multi-layered approach involving public education, regulatory enforcement, safe removal practices, and continual evaluation and refinement of safety protocols.
Public Education and Awareness:
Fundamental to minimizing asbestos-related risks is the bolstering of public awareness about the potential harms of asbestos exposure. Educational campaigns tailored toward homeowners, school administrators, and those in occupational settings where asbestos might be present are pivotal. Such campaigns should aim to elucidate the identification of asbestos-containing materials, the health risks associated with disturbing these materials, and the proper procedures for handling or reporting potential asbestos exposure.
Regulatory Measures and Compliance:
It is incumbent upon governments and regulatory bodies to establish stringent regulations concerning the use, abatement, and disposal of asbestos. This entails the strict prohibition of asbestos in new construction materials and the enforcement of comprehensive asbestos management plans for buildings that currently contain it. Periodic inspections and adherence to regulations regarding the removal and encapsulation are critical steps. Moreover, there should be stringent penalties for non-compliance, ensuring that the health and safety of individuals are not compromised by negligence.
Asbestos Abatement and Safe Removal:
Those engaged in asbestos abatement operations must adhere to the highest standards of safety and utilize state-of-the-art equipment and techniques. This includes the use of appropriate personal protective equipment (PPE), controlled wetting of asbestos to reduce airborne fiber release, and employing negative pressure environments to contain the fibers within designated areas. Post-abatement clearance testing should be mandatory to substantiate that an area is safe for reoccupation.
Occupational Safety:
Workers likely to encounter asbestos, such as those in construction, demolition, and maintenance, should be endowed with comprehensive training on safe working practices. Close adherence to Occupational Safety and Health Administration (OSHA) standards, which delineate safety requirements, is indispensable. Utilization of respiratory protection, decontamination procedures, and medical surveillance programs are essential components of shielding workers from asbestos exposure.
Advancements in Surveillance and Monitoring:
Surveillance systems tasked with identifying industries and occupations at high risk for asbestos exposure serve as an alarm system for early intervention. These systems can facilitate the timely updating of safety policies and pinpoint the need for additional training or resources in specific sectors.
Ongoing Research and Policy Evaluation:
To forestall future health complications linked to asbestos, there must be a sustained commitment to research. This dedication is paramount both in understanding the health risks associated with low-level and non-occupational exposures, and in refining preventative strategies. Policy evaluation is a continuous necessity, requiring the review of existing regulations, guidelines, and compliance to ensure that they are in concert with the current scientific consensus.
In summary, the alleviation of asbestos-related dangers will only be feasible through a synergistic blend of education, regulation, and vigilance.
Strategic oversight in policy enforcement, coupled with a foundation of research and continuous improvement, is paramount in safeguarding public health from the menaces of asbestos exposure.

Armed with an enhanced understanding of the pathogenic pathways triggered by asbestos, the latest advances in diagnostic methodologies, and an arsenal of existing and emerging therapeutic interventions, the medical community is better positioned to confront the challenges posed by asbestos exposure. While endeavoring to eradicate the specter of asbestos from our environment remains an ongoing battle, the diligent work of researchers and healthcare practitioners worldwide offers a beacon of hope. By diligently adhering to the rigorous standards of risk management and prevention, we fortify our collective resolve to shield future generations from the scourge of asbestos, steadfast in our commitment to safeguard public health and wellbeing.