Asbestos, once hailed as a wonder material for its fire-resistant properties, has been unveiled as a double-edged sword with lasting impacts on human health. As the general public, it is imperative to comprehend the complex pathophysiology of asbestos exposure—the quiet havoc it wreaks on biological tissues and the serious health conditions it can precipitate. This essay intends to unravel the sophisticated interplay between asbestos fibers and human physiology, shedding light on the inflammatory processes, cellular damage, and the ominous potential for cancerous transformations. By delineating the intricacies of disease manifestations, the rigors of diagnostic procedures, and scrutinizing the arsenal of current treatments, we sail on a voyage through the murky waters of asbestos-related medical interventions and preventative strategies, all within the reach of a society armed with knowledge to safeguard its members.
Pathophysiology of Asbestos Exposure
The Adverse Effects of Asbestos on Human Physiology
The silent but perilous risks posed by asbestos exposure remain a topic of significant concern within the scientific and medical communities. Asbestos, a term that references a group of minerals composed of microscopic fibers, was once widely used for its admirable resistance to heat, electricity, and corrosion. However, the revelation of its deleterious impact on human physiology has led to stringent regulation of its use and ongoing research into its health implications.
Central to understanding how asbestos exposure affects the human body is the mechanism by which these fibers interact with biological tissues. When asbestos-containing materials are disturbed, microscopic fibers are released into the air. Once inhaled, these fibers can penetrate deep into the lung tissue and even traverse into the pleura—the thin membrane lining the chest cavity and enveloping the lungs.
The human body struggles to expel these inhaled fibers, leading to inflammatory responses as a primary physiological consequence. Inflammation is the body’s innate reaction to foreign entities, yet chronic inflammation due to persistent asbestos fibers disrupts normal cellular function and can instigate further physiological complications.
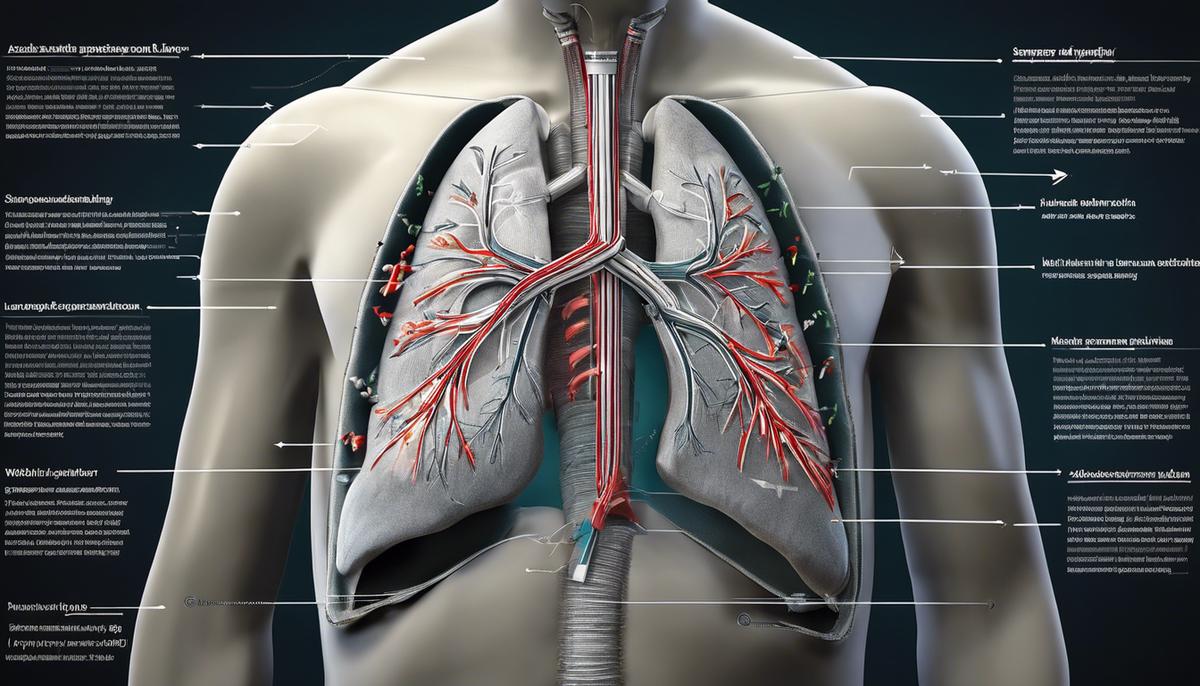
A hallmark condition associated with asbestos exposure is asbestosis, a progressive pulmonary disease characterized by scarring of lung tissue (fibrosis). As fibrosis advances, lung elasticity declines, culminating in diminished respiratory function. Individuals afflicted with asbestosis often suffer from symptoms such as persistent coughing, shortness of breath, and in severe cases, heart complications owing to increased strain on the pulmonary circuit.
Beyond asbestosis, asbestos exposure significantly elevates the risk of developing malignant mesothelioma—a rare and aggressive cancer predominantly affecting the pleura. Mesothelioma’s insidious nature lies in its protracted latency period; symptoms may not surface until decades post-exposure. Moreover, this cancer’s prognosis remains grim due to its typically advanced stage upon diagnosis.
It is also noteworthy that asbestos exposure can increase the likelihood of lung cancer, a condition not exclusive to smokers. Furthermore, asbestos has been linked to cancer of the larynx and ovaries, though the causal mechanisms necessitate further elucidation.
In preventative measures, numerous countries have mandated the removal of asbestos from buildings and industrial applications, and there is ongoing research into improved diagnostic and treatment options for asbestos-related diseases. Yet, the legacy of asbestos persists as current and past exposures continue to present significant health challenges.
Understanding the impact of asbestos on human physiology extends beyond the academic pursuit—it is a clarion call for continued vigilance, public health endeavors, and compassionate care for those bearing the burden of its lasting effects.

Disease Manifestations of Asbestos Exposure
Clinical manifestations resulting from asbestos exposure are broad-ranging and significantly impact respiratory health. Following the entry of asbestos fibers into the lungs, patients may exhibit pleural abnormalities. These are changes that occur in the pleura, which is the thin membrane enveloping the lungs and lining the chest cavity. Pleural plaques, for example, are discrete fibrous or partially calcified thickened areas that can be detected on chest X-rays. They are often asymptomatic but serve as markers of exposure.
Another consequence of asbestos inhalation is the development of pleural effusions, a condition where excess fluid accumulates in the pleural space, potentially causing discomfort and impaired breathing. Although effusions may resolve, recurrent episodes are common and can lead to pleural thickening or fibrosis, further constricting lung function.
Diffuse pleural thickening, characterized by extensive fibrosis, can encase the lung and significantly restrict lung expansion, resulting in breathlessness. This breathlessness is typically exertional at first but may progress to being present at rest in severe cases.
It is also important to note that individuals who have been exposed to asbestos may exhibit symptoms that mimic other respiratory conditions, thus complicating diagnosis. Clubbing of the fingers, or the enlargement of fingertips accompanied by changes under the nail beds, is one such symptom that might be observed. While clubbing is not exclusive to asbestos exposure and can be indicative of various types of lung damage, it is a potential sign of ongoing respiratory pathology tied to asbestos.
Moreover, asbestos exposure has been linked to the exacerbation of pre-existing respiratory conditions, notably obstructive lung diseases such as chronic obstructive pulmonary disease (COPD). In individuals with a history of asbestos exposure, COPD may manifest with increased severity, and the underlying scarring may impose added difficulties in disease management.
The recognition of these manifestations is vital for the early detection and intervention of asbestos-related diseases, as the progression and severity of these conditions can vary widely among exposed individuals. Screening and vigilant monitoring of those with known exposure remain critical components in mitigating the long-term health effects of this hazardous material. Continued education and awareness are imperative for clinicians and those at risk to navigate the challenges posed by the clinical ramifications of asbestos exposure.
Diagnostic Procedures for Asbestos-Related Diseases
The Focus on Diagnostics: Detecting Asbestos-Related Diseases
Advancements in medical diagnostics play a critical role in addressing the deleterious consequences of asbestos exposure. The critical window for intervention necessitates robust methods for the earliest possible detection of asbestos-related diseases. This discourse elucidates upon the diagnostics currently utilized in the detection of these pathological states.
Chest Radiography
remains the most accessible and widely utilized imaging modality in the initial assessment of individuals with suspected asbestos-related disease. Radiographic evidence can reveal irregularities suggestive of asbestosis, such as lower lung field opacities. However, its sensitivity is limited and more subtle forms of asbestos-related pathology may elude detection.
High-Resolution Computed Tomography (HRCT)
is integral in detecting fine detail not appreciated on chest X-rays. HRCT is adept in visualizing the patterns of lung parenchymal and pleural alterations distinctive of asbestos exposure, including honeycombing, ground-glass opacities, and herringbone patterns. It is particularly important in delineating the extent of pleural plaques and ascertaining the presence of pleural mesothelioma, a malignancy with a strong link to asbestos.
Pulmonary Function Tests (PFTs)
assess the mechanical function of the lungs. A reduction in lung volumes, particularly the forced vital capacity (FVC), and a decrease in total lung capacity (TLC), are indicative of restrictive lung disease which may arise from interstitial fibrosis due to asbestos. These tests are useful for both diagnostic and monitoring purposes.
Biomarkers
,while not definitive for asbestos-related diseases, provide additional information that can support a diagnosis when combined with imaging and clinical findings. Soluble mesothelin-related peptides (SMRP), for example, can be elevated in individuals with mesothelioma. Osteopontin is another biomarker under study for its potential to indicate exposure and disease.
Bronchoscopy with bronchoalveolar lavage (BAL)
can be conducted in cases where diagnostic uncertainty persists. While not specific for asbestos-related diseases, BAL may reveal inflammatory cells or allow for cytologic analysis that could help exclude other conditions.
Histopathological Examination
through biopsies of lung tissue, when clinically indicated, provides the most definitive diagnosis. These tissue samples can show the presence of asbestos bodies and fibrotic changes consistent with asbestosis or malignancy.
In summary, the diagnosis of asbestos-related diseases necessitates an integrative approach combining patient history, clinical examination, and an arsenal of diagnostic tests. Each aids in constructing a comprehensive picture of the individual’s health status, enabling tailored interventions and ongoing vigilance. The refinement of these diagnostic tools remains an area of dynamic research, underpinning the commitment to ameliorating the burden of asbestos-related morbidity and mortality.

Current Treatments for Asbestos-Related Conditions
Effective Management of Asbestos-Induced Illnesses: Current Therapeutic Strategies
Addressing the severe health ramifications of asbestos exposure necessitates a comprehensive and multi-faceted approach. With the disease burden inextricably linked to the deleterious nature of these mineral fibers, it is incumbent upon medical professionals to tailor treatment regimens that ameliorate symptoms and, where possible, attenuate the progression of illness.
Central to the management of asbestosis, a slowly progressive and incurable fibrotic lung disease, is the alleviation of respiratory distress. Supplemental oxygen therapy plays a pivotal role in this endeavor, enhancing the quality of life for individuals facing compromised pulmonary function. Concurrently, pulmonary rehabilitation programs are implemented to bolster patients’ physical conditioning and fortify respiratory muscle performance.
Moving over to the realm of oncology, malignant mesothelioma and asbestos-related lung cancers present with a daunting prognosis, thus garnering considerable therapeutic rigor. Chemotherapy remains the foundational treatment modality, with specialized drugs such as pemetrexed and cisplatin extending survival and palliating symptoms.
Recent advances have heralded the advent of targeted therapies—such as Bevacizumab, an angiogenesis inhibitor, which, when coupled with chemotherapy, has shown to improve outcomes in mesothelioma treatment. Immunotherapy has also emerged as a promising avenue of care, leveraging the body’s immune system to combat cancer cells, with agents like pembrolizumab receiving approval for certain subsets of patients.
Radiation therapy, too, occupies a notable place in treating these malignancies, either as a standalone treatment or in conjunction with surgical and medical interventions to optimize efficacy. Precise techniques such as Intensity-Modulated Radiation Therapy (IMRT) allow high doses to be focused on cancerous tissues while sparing adjacent healthy structures.
Surgery, while not universally applicable, offers hope for eligible candidates in the form of procedures like pleurectomy, decortication, or extrapleural pneumonectomy. These methods, while radical, may effectively remove diseased tissue and provide symptom relief.
Additionally, symptomatic treatments, including analgesics for pain and thoracentesis for pleural effusions, are also critical for managing the disease on a daily basis. The importance of mental health support for those affected and their families cannot be overstated, as the psychological toll of chronic illnesses is substantial.
Finally, the development and optimization of multidisciplinary care teams that provide personalized care plans remain critical in advancing the management of asbestos-induced diseases. It is through the lens of individual patient needs and the nuances of their disease manifestations that treatments continue to evolve, faithfully reflecting the complexity and individuality of each case.
While this is not an exhaustive survey of all treatment strategies, it encompasses the focal pillars currently deployed in the management of asbestos-induced conditions. As research continues to unravel the myriad aspects of these diseases, the therapeutic landscape will, undoubtedly, broaden, refining our ability to confront the challenges posed by asbestos with even greater precision and effectiveness.

Preventative Measures and Asbestos Regulations
Asbestos, a naturally occurring fibrous mineral, historically exploited for its insulating and fire-resistant properties, poses significant health risks upon exposure. Understanding these risks, regulatory entities have established a framework of preventative measures designed to mitigate asbestos exposure and shield public health.
Occupational Safety and Health Administration (OSHA) and Environmental Protection Agency (EPA) in the United States enforce strict regulations concerning asbestos management. For example, the OSHA Asbestos Standards (29 CFR 1910.1001 and 1926.1101) delineate permissible exposure limits (PELs) in workplace air over an 8-hour time-weighted average, along with compulsory practices for monitoring and reporting. Industries traditionally at risk, such as construction and shipyard sectors, must comply with exacting safety protocols, including the provision of personal protective equipment (PPE), to prevent inhalation or ingestion of asbestos fibers.
Further, the EPA’s National Emission Standards for Hazardous Air Pollutants (NESHAP) regulate the renovation, demolition, and disposal of buildings containing asbestos. These regulations ensure that asbestos materials are properly handled and disposed of to avoid releasing fibers into the air, by mandating the use of wetting agents during abatement activities and the containment of renovation sites.
Building codes and regulations also contribute to preventing asbestos exposure in new structures. The adoption of asbestos-free materials in construction is now standard, significantly curtailing the potential for exposure in modern buildings.
Preventative measures extend into public health initiatives, such as periodic air quality monitoring in areas with natural asbestos deposits or legacy asbestos products. Community awareness programs inform residents about the risks of asbestos exposure and best practices for avoiding contact with contaminated sites or materials.
Educational efforts, particularly in the realm of occupational health, focus on imparting knowledge on the proper use of PPE, decontamination procedures, and the significance of adhering to established safety guidelines. Training courses for asbestos abatement professionals aim to ensure that workers understand the nature of the hazard and the necessity of rigorous controls to prevent exposure.
Moreover, asbestos exposure regulations include requirements for posting clear signage in areas where asbestos-related activities are performed, informing all personnel of the potential danger and necessary safety precautions.
With these multifaceted preventative measures and stringent regulatory standards, the cumulative efforts of government, industry, and public health organizations serve to protect society from the enduring threat posed by asbestos. The culmination of these endeavors results in an environment where the likelihood of exposure is considerably diminished, thus preserving both individual health and the well-being of the broader community.

Photo by selimarda on Unsplash
Emerging Research and Future Directions
The nexus of medical science and toxicology is continually expanding, offering fresh insights into combating the ill effects of hazardous substances. Asbestos, a notorious agent once ubiquitous in the construction industry, falls within this sphere of concern. Future prospects in medical interventions for asbestos exposure promise a convergence of innovation and interdisciplinary strategies.
Given the intractable nature of asbestos-related diseases (ARDs), the pursuit of novel therapeutics is a paramount concern. Gene therapy has entered the arena as a promising frontier. Emerging research suggests that genetic interventions may one day repair or mitigate the cellular damage wrought by asbestos fibers, potentially reversing the progression of conditions like asbestosis.
Another developing area is the concept of chelation therapy, which has been used effectively for heavy metal poisoning. It is postulated that asbestos fibers may bind with certain molecules that can be targeted and neutralized by chelating agents, thereby facilitating the removal of fibers from the lung tissue.
The role of anti-fibrotic drugs, which have shown promise in treating other fibrotic diseases, is being examined for their potential to halt or slow the fibrotic process in patients with asbestosis. Agents such as pirfenidone or nintedanib represent a ray of hope for those with progressive fibrosis.
The realm of immune modulation also presents a fertile ground for intervention. Given the immune dysregulation observed in ARDs, vaccines are being studied, which may harness the body’s immune response to fight the onset of diseases like mesothelioma.
Precision medicine is tailor-making therapies based on individual genetic profiles, and biomarker discovery is key to this strategy. Identifying specific biomarkers linked to asbestos exposure and disease progression enables the development of targeted therapies that can specifically address individual patient pathologies.
Stem cells and regenerative medicine hold potential for repairing damaged lung tissue, with preclinical studies showing that stem cells can modulate inflammation and promote healing. The implications for asbestosis and other chronic lung conditions are significant, with the prospect of not merely slowing but restoring lost lung function.
Technology also plays a pivotal role. Wearable tech for continuous health monitoring may offer real-time data on lung function and biomarker levels, allowing for immediate intervention at the earliest signs of disease exacerbation. Telemedicine is anticipated to expand care access, particularly for patients in remote or underserved locations that historically handled asbestos and may have higher incidences of ARDs.
Lastly, the intersection of artificial intelligence (AI) with medicine is set to revolutionize diagnostics and treatment planning. Advanced algorithms can integrate vast datasets from clinical, imaging, and molecular diagnostics, yielding unparalleled precision in disease prediction and management strategies.
In conclusion, the horizon glimmers with the promise of breakthroughs in the fight against asbestos-induced disease. Hindering the threat posed by this silent scourge necessitates a vanguard approach, one where science’s clarion call animates the relentless quest for novel interventions. With collective vigilance and adroit application of advancing technology, the scourge that asbestos represents will hopefully one day be relegated to the annals of occupational health hazards, subdued by the tireless march of medical endeavor.

The safety and well-being of individuals in the face of hazardous substances like asbestos hinge upon our collective efforts to remain vigilant, informed, and proactive. By threading together the latest advancements in medical research with steadfast public health policies, we pave the way towards a future less burdened by the legacy of asbestos exposure. As we continue to challenge the frontiers of scientific inquiry and refine our approach to policy-making, the hope for more effective preventative measures, refined diagnostic tools, and revolutionary treatments glimmers on the horizon. Ensuring that this wealth of knowledge translates into tangible benefits for those at risk or afflicted by asbestos-related diseases is not just a professional mandate; it is a moral imperative that transcends the confines of academia and resonates within the heart of our community.